Technology
Orthopaedic Surgery is a field that is constantly advancing to better address the problems facing its patients. This evolution is perhaps best evidenced through recent advances in total joint arthroplasty. The materials that we utilize for implants have changed dramatically in the last 20 years and have allowed for more durable joint replacements with longer survivorship. Adjunctive technology including computer software and navigation has allowed for more accurate sizing and placement of these implants as well.
Furthermore, other materials and strategies are constantly being developed to reduce the rates of perioperative complications such as infection and accelerate functional recovery. This portion of my website is dedicated to showcasing these technological advances and their application in my practice.
Hip Arthroplasty
Hip Arthroplasty implant selection is an art. Considerable time and thought is devoted to each patient during this selection process, as femoral geometry, size, and bone quality are radiographically assessed and matched to the ideal implant. As such, a variety of stem options are employed in my practice. These stem options include stems manufactured by Smith and Nephew (Anthology, Polar, Redapt, Spectron), Zimmer/Biomet (MLT, Echo Microplasty, Versys Heritage), and DePuy (S-ROM).
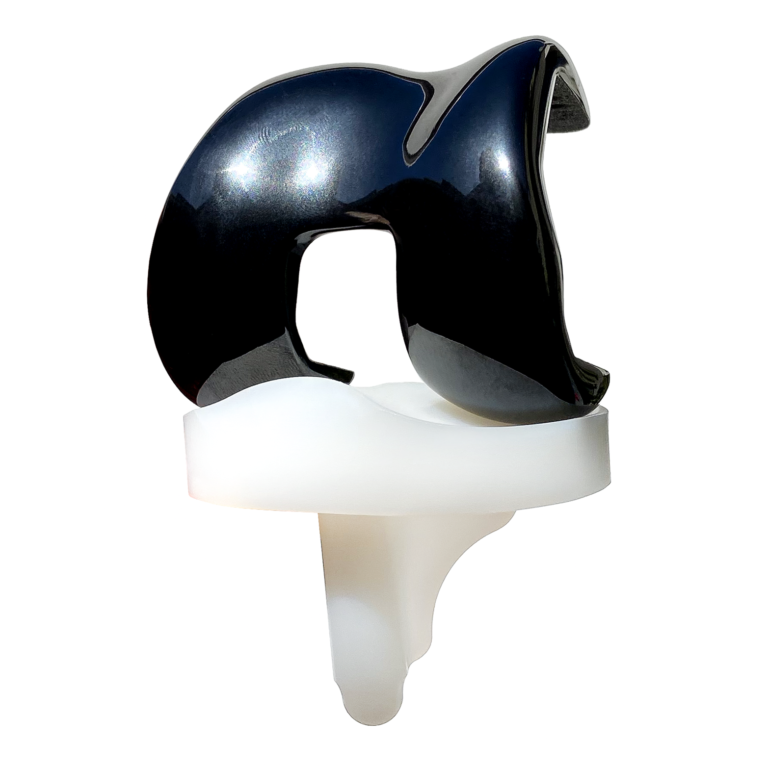
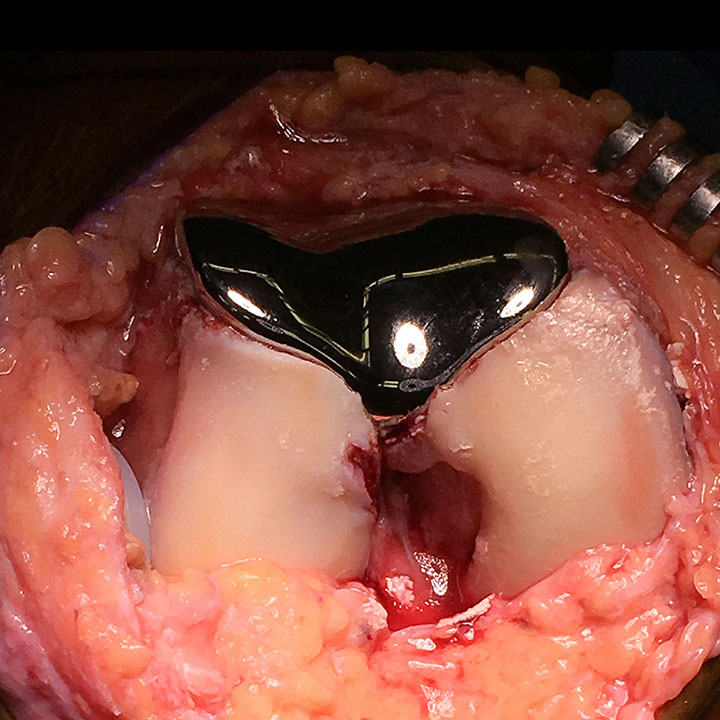
The acetabular component (socket implant) has less variation and is typically selected based on bone quality, the need to manage any acetabular defects, and the presence of dysplasia. Almost uniformly, the acetabular components I use are composed of porous titanium alloy to enhance bony ingrowth and achieve long lasting fixation. The bearing couple I employ is dependent on the stability of the joint. Typically standard bearing couples are utilized, composed of Oxinium or Biolox Delta ceramic femoral head components and highly cross-linked polyethylene acetabular liners. Some patients may require increased stability or have a higher demand on range of motion following their hip replacement. In these instances a dual mobility bearing is typically utilized to allow for a larger femoral head size.
In the revision hip replacements, bone loss is frequently encountered and is usually managed with longer stemmed femoral components. Revision hip arthroplasty may also require socket augmentation with either porous metal augments or cadaveric bone grafting.
Total Knee Arthroplasty
For my total knee arthroplasty procedures, I use the Smith and Nephew Legion system. I typically combine an all-polyethylene tibial component with an Oxinium femoral component. I prefer this system as it has a long track record based on registry data with excellent survivorship.
Oxinium is an oxidized zirconium that has improved wear characteristics (less debris generated with joint motion) and is biologically inert (your body does not react negatively to it). It also does not expose my patients to any cobalt, nickel, or chromium ions that may be released from other implants on the market.
Finally the survivorship of all-polyethylene tibial components has been shown to be superior to metal backed implants.
Unicompartmental Knee Arthroplasty
For my unicompartmental knee arthroplasty procedures, I use Smith and Nephew Journey Oxinium Femoral components with ZUK all-polyetheylene tibial components. This is due to the long track record and demonstrated excellent survivorship of the ZUK tibial component, and the ability to mate this to an Oxinium femoral component. Similar to my philosophy in selecting total knee implants, these partial knee implants decrease any potential risk for adverse local tissue reactions to metal debris.
Patellofemoral Arthroplasty
For my patellofemoral arthroplasty procedures, I utilize the Zimmer/Biomet patellofemoral replacement system. This system’s milling technique in conjunction with its onlay design that incorporates an increased trochlear groove angle facilitates a reproducible procedure, optimal patellar tracking, and tailored implant selection.
Revision Total Knee
Arthroplasty
Revision knee arthroplasty can be technically challenging because of the difficulty incurred in removing previous implants and managing the bone loss following their removal. Moreover, the ligamentous stability of the knee may often be compromised and soft-tissue balancing may be difficult to achieve.
I use the Smith and Nephew Legion Revision System for the vast majority of my revision knee arthroplasty procedures. It is a comprehensive system that allows for enhanced fixation via metaphyseal cones, offset couplers, augments, and stems. Additionally, varied levels of constraint, including hinged implants, can be employed to ensure adequate joint stability is achieved.
Computer Navigation
Computer Navigation is a developing tool within total joint replacement that can enhance the accuracy of implant positioning and may lead to improved clinical outcomes. There are multiple platforms for navigation currently available. OrthAlign, which is a accelerometry guided system, is the navigation system I use most commonly given its proven track record, ability to be used with any implant system, and seamless integration into current total joint replacement techniques. This navigation can be applied to partial knee replacements, total knee replacements, and total hip replacements.
Please, view the video below and watch me use the OrthAlign navigation system during a total knee arthroplasty.
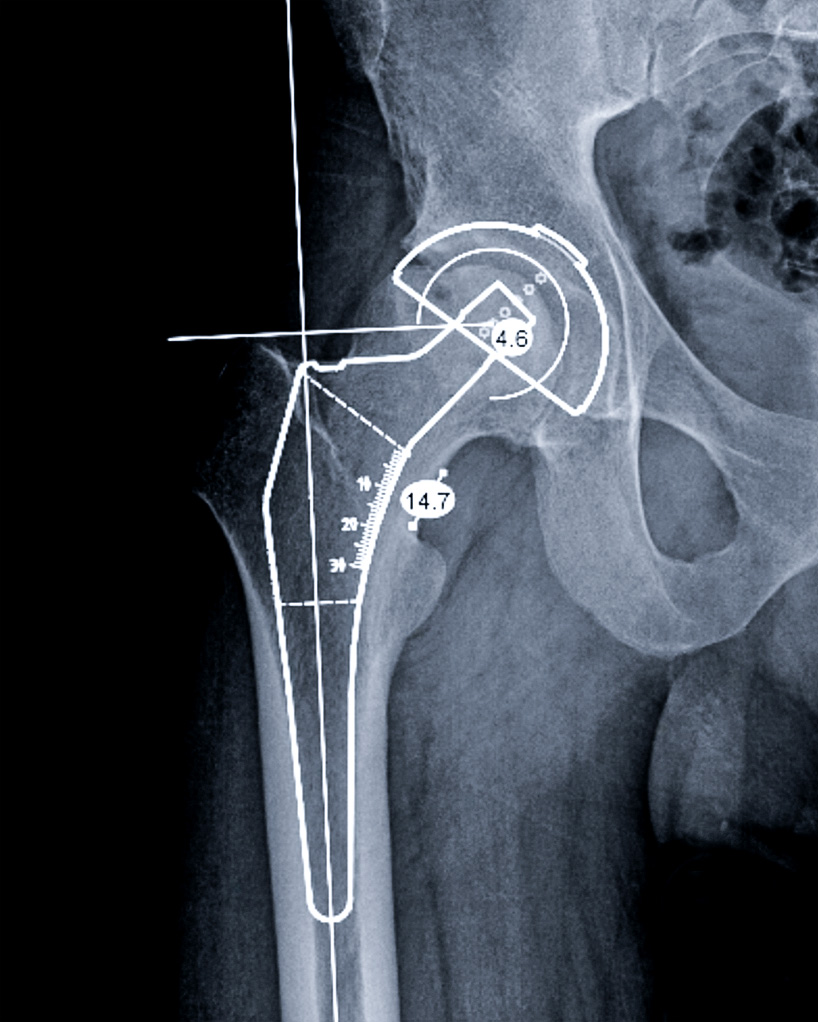
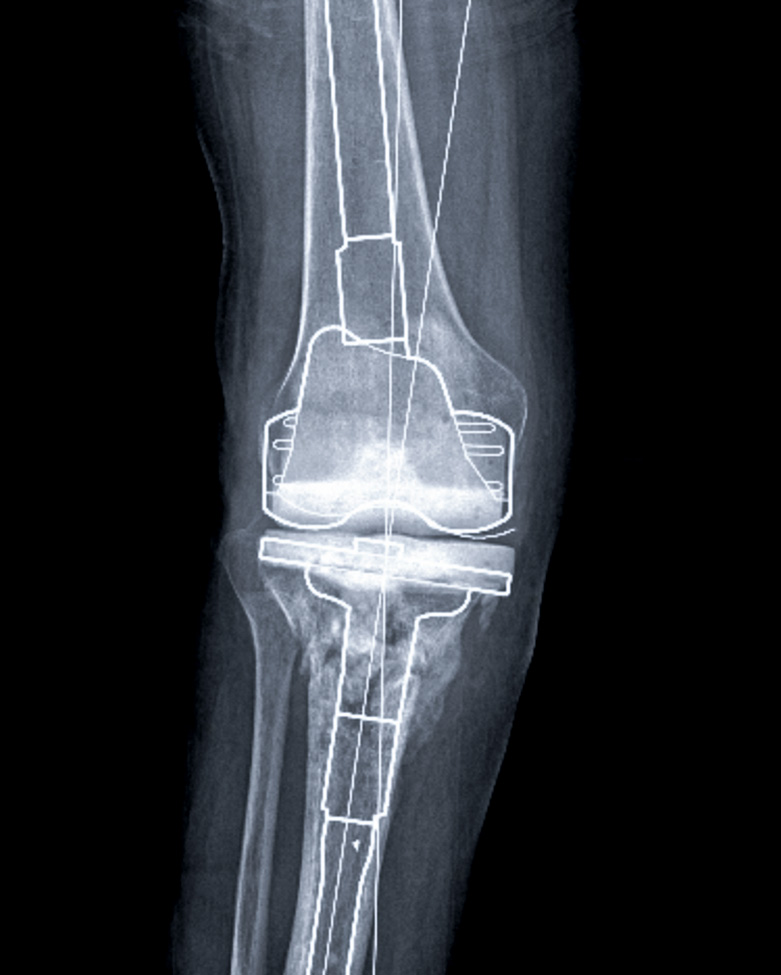
Templating
Software
Prior to physically performing your surgery, it is performed virtually. Templating software is used to plan bony resections and allows us to overlay implants on your X-rays, so that the proper sizes are anticipated. This allows for more accurate restoration of joint and limb alignment and helps ensure surgical excellence.

Advanced Recovery Protocol

Total Joint Arthroplasty has progressed tremendously during the last decade. The vast majority of these clinical improvements have been centered on advanced recovery protocols and accelerated return to function following surgery. Currently, the majority of patients undergoing partial knee replacements, total knee replacements, and total hip replacements can return home the day of surgery. This is facilitated by our strong partnership with the anesthesiology department and use of regional blocks in conjunction with a spinal anesthetic as the gold standard of care for the majority of cases. Additionally, a multi-modal pain control pathway is used to limit post-operative narcotic consumption while enabling post-operative recovery.
Returning to your home the day of surgery is important in decreasing your risk of infection by limiting contact with other potentially sick patients in the hospital. It also affords you with a quicker transition to the comforts of home and outpatient physical therapy. Orchestrating this transition home takes a great deal of care coordination on the part of the surgical team, anesthesiologists, nursing staff, physical/occupational therapists and the patient. Ideally, the patient has a “care partner” that can help them at home for the first few days following surgery. Usually this care partner is a spouse, domestic partner, other family member, or close friend.
We encourage our patients and their care partners to attend a pre-operative class together, in person or online, so they are familiar with the expected proceedings on the day of their procedure and during their first few days at home following surgery. Online classes are available for your viewing via these links:
Infection
Prevention
Infection following total joint arthroplasty is a dreaded complication. As such great care and considerable effort is aimed at preventing this complication. Special soap is used prior to your joint replacement, meticulous sterile technique is used during your procedure, and special dressings are utilized to maintain a local sterile environment while your wound heals. Additionally if you are deemed to have a higher risk for a postoperative infection (revision procedures, poorly controlled diabetes, obesity, immunocompromised, etc.) adjunctive measures may be employed to help mitigate this increased risk.
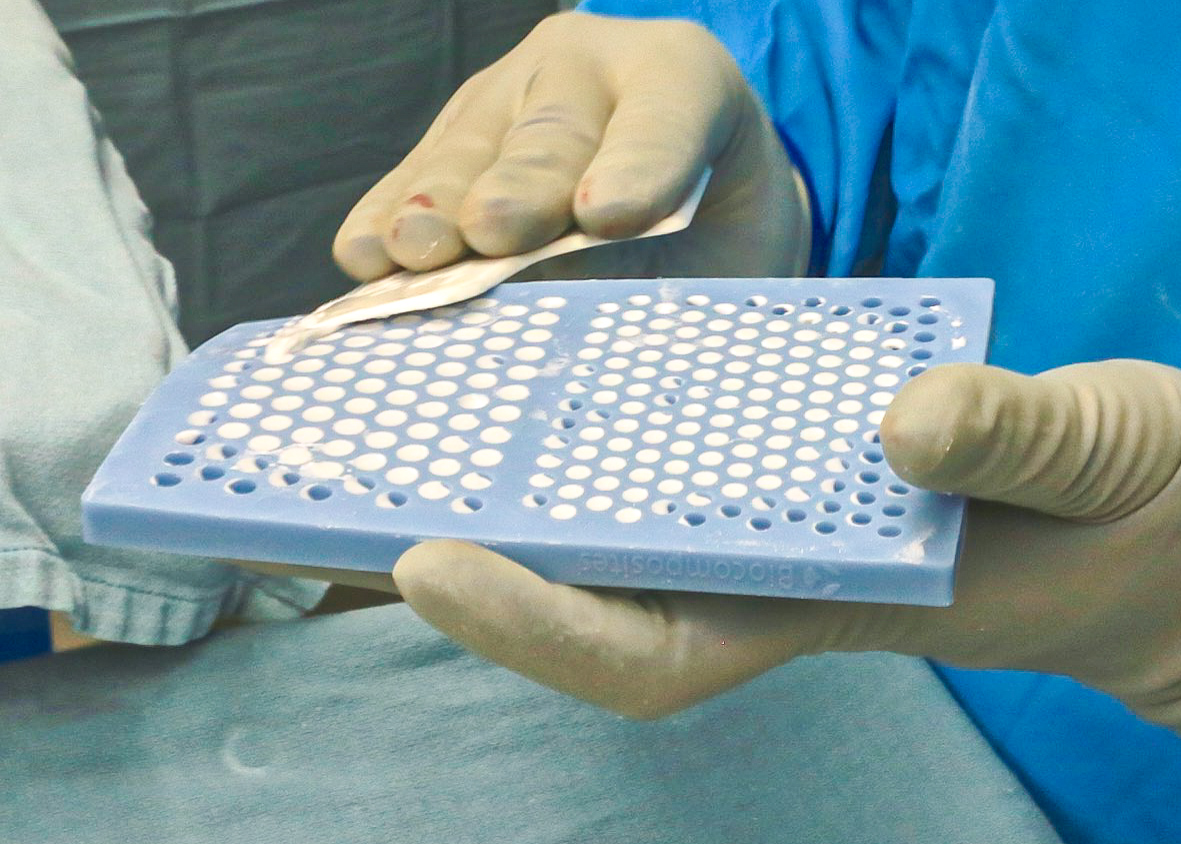
One such measure includes the creation of Stimulan, antibiotic eluting, calcium sulfate beads, which are placed in the surgical field prior to closure. This beads gradually dissolve, giving off high doses of local antibiotics to protect your joint replacement from bacteria, especially in the setting of delayed wound healing.




Negative pressure dressings are another frequently used tool in my practice and help seal your wound from the outside environment, while applying a gentle vacuum pressure to the skin. This facilitates healing and blood flow, while reducing surface moisture and local swelling. These dressings may stay on for 1-2 weeks at a time thereby decreasing risks of wound contamination that may be encountered with frequent dressing changes.